
Background: Splenectomy is an effective second line therapy for patients with immune cytopenias. Fifteen percent of patients are going to relapse after splenectomy. These patients are categorized as refractory and their treatment is challenging. The incidence of an accessory spleen diagnosed by gammagraphy is estimated to be 8-20% in this scenario. Current treatment guidelines do not address the issue of searching for an accessory spleen or performing accessory splenectomy as a treatment strategy for these patients.
The aim of this study was to identify risk factors for the presence of accessory spleen diagnosed by gammagraphy in patients with refractory immune cytopenias and analyze the response rate of its removal.
Methods: It is a case control, single center, retrospective study. We included adult patients with refractory immune cytopenias who underwent gammagraphy to search for an accessory spleen, from 1996 to 2016. Cases were patients with a positive gammagraphy, controls were those with a negative gammagraphy. Patients who failed to have at least one year of follow-up after splenectomy or accessory splenectomy, were excluded. A logistic regression was performed to determine factors associated with the presence of an accessory spleen.
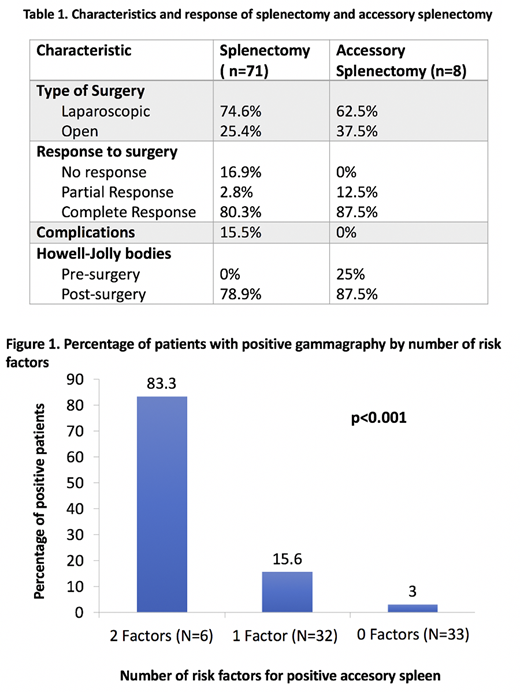
Results: We analyzed 71 refractory patients with a gammagraphy performed searching for an accessory spleen, 87.3% with a diagnosis of immune thrombocytopenia (IT), 7% autoimmune hemolytic anemia (AHA) and 5.6% Evans Syndrome. Fourteen percent of the patients had secondary immune cytopenias all of them due to autoimmune diseases. There was a predominance of women with 74.6% of the subjects studied. Patients received a median of 2 (0-4) lines of treatment before the splenectomy. The majority of patients (98.6%) had received, as first line of treatment corticosteroids, with an overall response rate (ORR) of 84% and a complete response (CR) rate of 38.6%. Of the 71 patients, splenectomy achieved an ORR of 83.1% with CR in 80.3%. The incidence of accessory spleen diagnosed by gammagraphy at their relapse was 15.5% (11 patients). In the multivariate analysis, we found two factors associated with positivity of the gammagraphy: CR to corticosteroids pre-splenectomy with an OR of 5.2 (CI 95% 1.24-21.78; p=0.021) and the presence of Howell Jolly bodies (HJb) with an OR of 0.088 (CI95% 0.02-0.37; p=0.001) as a protective factor. We developed a risk score consisting of: 0 risk factors, 1 risk factor (CR to corticosterois pre-splenectomy or abscense of HJb) and 2 risk factors. The percentage of patients who were positive by gammagraphy using this score was 83.3%, 25.6% and 3% for 2, 1 and no risk factors respectively (p<0.001) (Figure1). Eight patients underwent accesory splenectomy, all of them achieved responses with CR of 87.5%, and none experienced complications associated with the procedure. Seven patients acquired the presence of HJb after accesory splenectomy (Table 1). With a median follow-up of 60.2 months (1.54-194.56), 62.5% mantained the response obtained with the accesory splenectomy. One patient didn´t acquire HJb post accesory splenectomy, he relapsed and was diagnosed with a new accesory spleen. He underwent a second accesory splenectomy and is now in CR with the presence of HJb in the blood smear.
Conclusions: The search for an accesory spleen in patients with refractory immune cytopenias with risk factors (absence of Howell Jolly bodies and or complete response to steroids as first line therapy) is usefull. Accesory splenectomy is a safe and effective therapeutic strategy in the treatment of these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal